The relationship of Lysophosphatidylcholine level with mortality in Covid Pneumonia
DOI:
https://doi.org/10.51271/ajh.72Keywords:
COVID-19 pneumonia, Lysophosphatidylcholine levels, mortalityAbstract
INTRODUCTION: The aim of this study was to investigate the relationship between serum Lysophosphatidylcholine (LPC) levels and mortality in patients diagnosed with Covid-19 admitted to the emergency department and hospitalised.
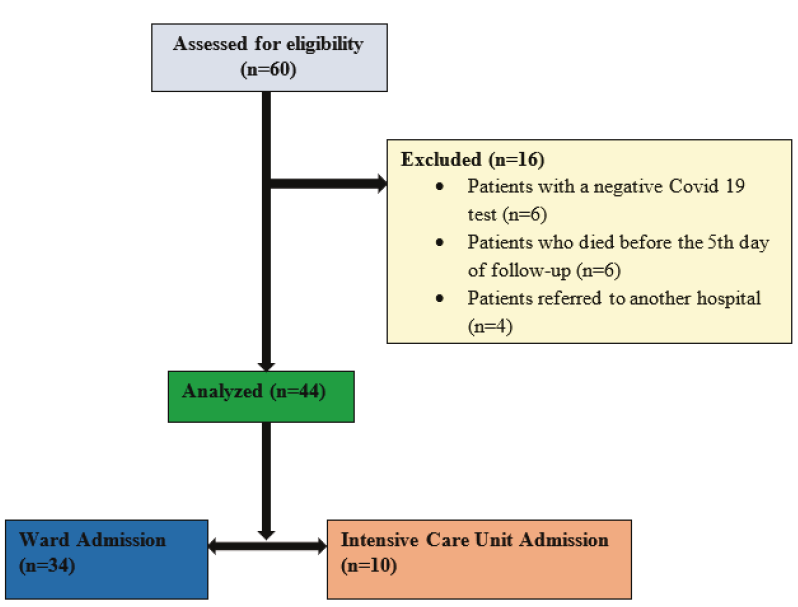
METHODS: The study was designed as a prospective, cross-sectional study. The effect of serum LPC levels taken on days 1 and 5 on prognosis in patients diagnosed with Covid 19 in the emergency department was investigated.
RESULTS: The average age of the patients included in our study was 73.9, with males constituting 56.8%. The most common comorbidities were hypertension (72.7%) and diabetes mellitus (43.2%). The most common presenting symptoms were fatigue and widespread body pain, cough, and dyspnoea, consistent with the cardinal symptoms of the disease. After the emergency department visit, 77.3% of the patients were hospitalized, while 22.7% were admitted to the intensive care unit. 79.5% were discharged, while 20.5% died. In the group with fatal outcomes, the day 1 LPC level was significantly lower (p < 0.05) compared to the discharged group. A significant [Area under the curve (AUC): 0.830; Confidence Interval (CI): 0.683-0.977)] effectiveness of the 10000-cut-off value of LPC on the 1st day was observed in distinguishing between patients discharged and deceased. The sensitivity was 88.9%, positive predictive value 50.0%, specificity 77.1%, and negative predictive value 96.4%.
DISCUSSION AND CONCLUSION: We found that the day 1 LPC level may be a valuable biomarker for prognosis in patients presenting to the emergency department with Covid pneumonia due to its high sensitivity, moderate specificity, and advanced negative predictive value for mortality.
References
Miesbach W, Makris M.COVID-19: Coagulopathy, Risk of Thrombosis, and the Rationale for Anticoagulation; Clinical and Applied Thrombosis/Hemostasis Volume 26: 1-7 The Author(s) 2020 DOI: 10.1177/1076029620938149.
Wilensky, R. L., Shi, Y. I., Mohler III, E. R., Hamamdzic, D., Burgert, M. E., et al. Inhibition of lipoprotein-associated phospholipase A2 reduces complex coronary atherosclerotic plaque development. Nature medicine, 14(10), 1059-1066. https://doi.org/10.1038/nm.1870
Bach, G., Perrin-Cocon, L., Gerossier, E., Guironnet-Paquet, A., Lotteau, V., Inchauspé, G., et al. Single lysophosphatidylcholine components exhibit adjuvant activities in vitro and in vivo. Clinical and Vaccine Immunology, 17(3), 429-438. https://doi.org/10.1128/CVI.00420-09
Lauber, K., Bohn, E., Kröber, S. M., Xiao, Y. J., Blumenthal, S. G., Lindemann, R. K., et al. Apoptotic cells induce migration of phagocytes via caspase-3-mediated release of a lipid attraction signal. Cell, 113(6), 717-730. https://doi.org/10.1016/S0092-8674(03)00422-7
Chavez-MacGregor, M., Lei, X., Zhao, H., Scheet, P., Giordano, S. H. Evaluation of COVID-19 mortality and adverse outcomes in US patients with or without cancer. JAMA oncology, 8(1), 69-78. doi:10.1001/jamaoncol.2021.5148
Biswas, M., Rahaman, S., Biswas, T. K., Haque, Z., Ibrahim, B. Association of sex, age, and comorbidities with mortality in COVID-19 patients: a systematic review and meta-analysis. Intervirology, 64(1), 36-47. https://doi.org/10.1159/000512592
Chavez, S., Long, B., Koyfman, A., & Liang, S. Y. (2021). Coronavirus Disease (COVID-19): A primer for emergency physicians. The American journal of emergency medicine, 44, 220-229. https://doi.org/10.1159/000512592
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The lancet, 395(10229), 1054-1062. https://doi.org/10.1016/S0140-6736(20)30566-3
Zhang, J. J., Dong, X., Cao, Y. Y., Yuan, Y. D., Yang, Y. B., Yan, Y. Q., et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy, 75(7), 1730-1741. https://doi.org/10.1111/all.14238
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The lancet, 395(10229), 1054-1062. https://doi.org/10.1016/S0140-6736(20)30566-3
Mudatsir, M., Fajar, J. K., Wulandari, L., Soegiarto, G., Ilmawan, M., Purnamasari, Y., et al. Predictors of COVID-19 severity: a systematic review and meta-analysis. F1000Research, 9. https://doi.org/10.12688%2Ff1000research.26186.2
Cho, W. H., Yeo, H. J., Yoon, S. H., Lee, S. E., Jeon, D. S., Kim, Y. S., et al. Lysophosphatidylcholine as a prognostic marker in community-acquired pneumonia requiring hospitalization: a pilot study. European Journal of Clinical Microbiology & Infectious Diseases, 34, 309-315. https://doi.org/10.1007/s10096-014-2234-4
Cho, W. H., Park, T., Park, Y. Y., Huh, J. W., Lim, C. M., Koh, Y., et al. Clinical significance of enzymatic lysophosphatidylcholine (LPC) assay data in patients with sepsis. European journal of clinical microbiology & infectious diseases, 31, 1805-1810. https://doi.org/10.1007/s10096-011-1505-6
Park, D. W., Kwak, D. S., Park, Y. Y., Chang, Y., Huh, J. W., Lim, C. M., et al. Impact of serial measurements of lysophosphatidylcholine on 28-day mortality prediction in patients admitted to the intensive care unit with severe sepsis or septic shock. Journal of critical care, 29(5), 882-e5. https://doi.org/10.1016/j.jcrc.2014.05.003
Cheng, L., Li, H., Li, L., Liu, C., Yan, S., Chen, H., et al. Ferritin in the coronavirus disease 2019 (COVID‐19): a systematic review and meta‐analysis. Journal of clinical laboratory analysis, 34(10), e23618. https://doi.org/10.1002/jcla.23618
Moradi, E. V., Teimouri, A., Rezaee, R., Morovatdar, N., Foroughian, M., Layegh, P., et al. Increased age, neutrophil-to-lymphocyte ratio (NLR) and white blood cells count are associated with higher COVID-19 mortality. The American journal of emergency medicine, 40, 11-14. https://doi.org/10.1016/j.ajem.2020.12.003
Khinda, J., Janjua, N. Z., Cheng, S., van den Heuvel, E. R., Bhatti, P., Darvishian, M.. Association between markers of immune response at hospital admission and COVID‐19 disease severity and mortality: a meta‐analysis and meta‐regression. Journal of medical virology, 93(2), 1078-1098. https://doi.org/10.1002/jmv.26411
Halaby, R., Popma, C. J., Cohen, A., Chi, G., Zacarkim, M. R., Romero, G., et al. D-Dimer elevation and adverse outcomes. Journal of thrombosis and thrombolysis, 39, 55-59. https://doi.org/10.1007/s11239-014-1101-6
Zhang, L., Feng, X., Zhang, D., Jiang, C., Mei, H., Wang, J., et al. Deep vein thrombosis in hospitalized patients with COVID-19 in Wuhan, China: prevalence, risk factors, and outcome.Circulation,142(2),114-128. https://doi.org/10.1161/CIRCULATIONAHA.120.046702
Velavan, T. P., & Meyer, C. G. Mild versus severe COVID-19: Laboratory markers. International Journal of Infectious Diseases, 95, 304-307. https://doi.org/10.1016/j.ijid.2020.04.061
Jickling, G. C., Montaner, J. Lysophosphatidylcholine to stratify risk of ischemic stroke in TIA. Neurology, 84(1), 17-18. https://doi.org/10.1212/WNL.0000000000001100
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Selen Dehmen, Adem Melekoğlu, Uğur Kahveci, Serkan Ceritli, Sema Yağcı, Ertuğrul Altınbilek

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.