Foot Drop as an Atypical Presentation of Rectal Cancer: The Importance of Digital Rectal Examination in Early Diagnosis
DOI:
https://doi.org/10.51271/ajh.67Keywords:
Foot drop, Digital rectal examination, Rectal cancerAbstract
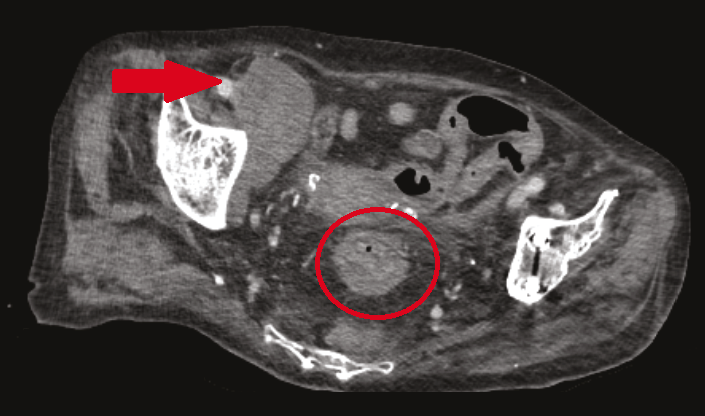
Rectal cancer is a major health concern with an increasing incidence in the younger population. It is typically diagnosed through screening or through common symptoms, such as rectal bleeding and changes in bowel habits. Rarely, rectal cancer may present with atypical symptoms such as neurological deficits. We report the case of a 77-year-old female with a history of abdominal pain and constipation, who presented with foot drop, a rare neurological manifestation. Clinical examination and imaging revealed an irregular mass in the rectum and metastatic lymphadenopathy. Digital rectal examination (DRE) plays a crucial role in identifying primary malignancies despite the absence of typical symptoms. The patient was diagnosed with moderately differentiated adenocarcinoma of the rectum, which was confirmed by colonoscopy and biopsy. Further staging with PET-CT revealed metastatic lymph nodes. Owing to obstructive symptoms, she underwent palliative loop sigmoid colostomy and started chemotherapy. This case highlights the importance of considering rare neurological presentations such as foot drop in the diagnosis of rectal cancer. Early recognition through DRE and imaging can lead to timely diagnosis and intervention, and improve patient outcomes.
References
International Agency for Research on Cancer. Global Cancer Observatory [Internet]. Lyon: IARC; [cited 2024 Apr 22]. Available from: https://gco.iarc.fr/en
Vogel JD, Felder SI, Bhama AR, Davids JS, Hawkins AT, Keller DS, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of colon cancer. Dis Colon Rectum. 2022;65(2):148–77. doi:10.1097/DCR.0000000000002323
Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019;14(2):89-103. doi: 10.5114/pg.2018.81072. Epub 2019 Jan 6. PMID: 31616522; PMCID: PMC6791134.
Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; CARE Group. The CARE Guidelines: Consensus-based Clinical Case Reporting Guideline Development. J Clin Epidemiol. 2014;67(1):46-51. doi:10.1016/j.jclinepi.2013.08.003).
Manisundaram NV, Buhutiani N, You NN. Cancer of the colon, rectum and anus. In: Faig BW, White MG, Gaskill CE, Kothari AN, DiBrito SR, editors. The MD Anderson Surgical Oncology Manual. 7th ed. Philadelphia: Wolters Kluwer; 2024. p. 278–331.
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625–38. doi:10.1056/NEJMoa021423
Farooq O, Farooq A, Ghosh S, Anthony T, Cosgrove J, Le P, et al. The digital divide: A retrospective survey of digital rectal examinations during the workup of rectal cancers. Healthcare (Basel). 2021;9(7):855. doi:10.3390/healthcare9070855
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17–48. doi:10.3322/caac.21763
Boysen AK, Ording AG, Astradsson A, Iversen LH, Nørrelund H, Cronin-Fenton D. Metastasis-directed treatment of brain metastases from colorectal cancer: a Danish population-based cohort study. Acta Oncol. 2020;59(9):1118–22. doi:10.1080/0284186X.2020.1769861
Felice KJ, Donaldson JO. Lumbosacral plexopathy due to benign uterine leiomyoma. Neurology. 1995;45(10):1943–4. doi:10.1212/WNL.45.10.1943
Jaeckle KA, Young DF, Foley KM. The natural history of lumbosacral plexopathy in cancer. Neurology. 1985;35(1):8–15. doi:10.1212/WNL.35.1.8
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Emre Tunç, Ferit Aydin, Toygar Sarı, Bülent Aksel, Lütfi Doğan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.