Antibiotic Susceptibilities of Escherichia coli and Klebsiella pneumoniae Isolates from Clinical Samples: 3-Year Analysis
DOI:
https://doi.org/10.14744/ajh.66Keywords:
Escherichia coli, ESBL, Klebsiella pneumoniae, Antibiotic susceptibilityAbstract
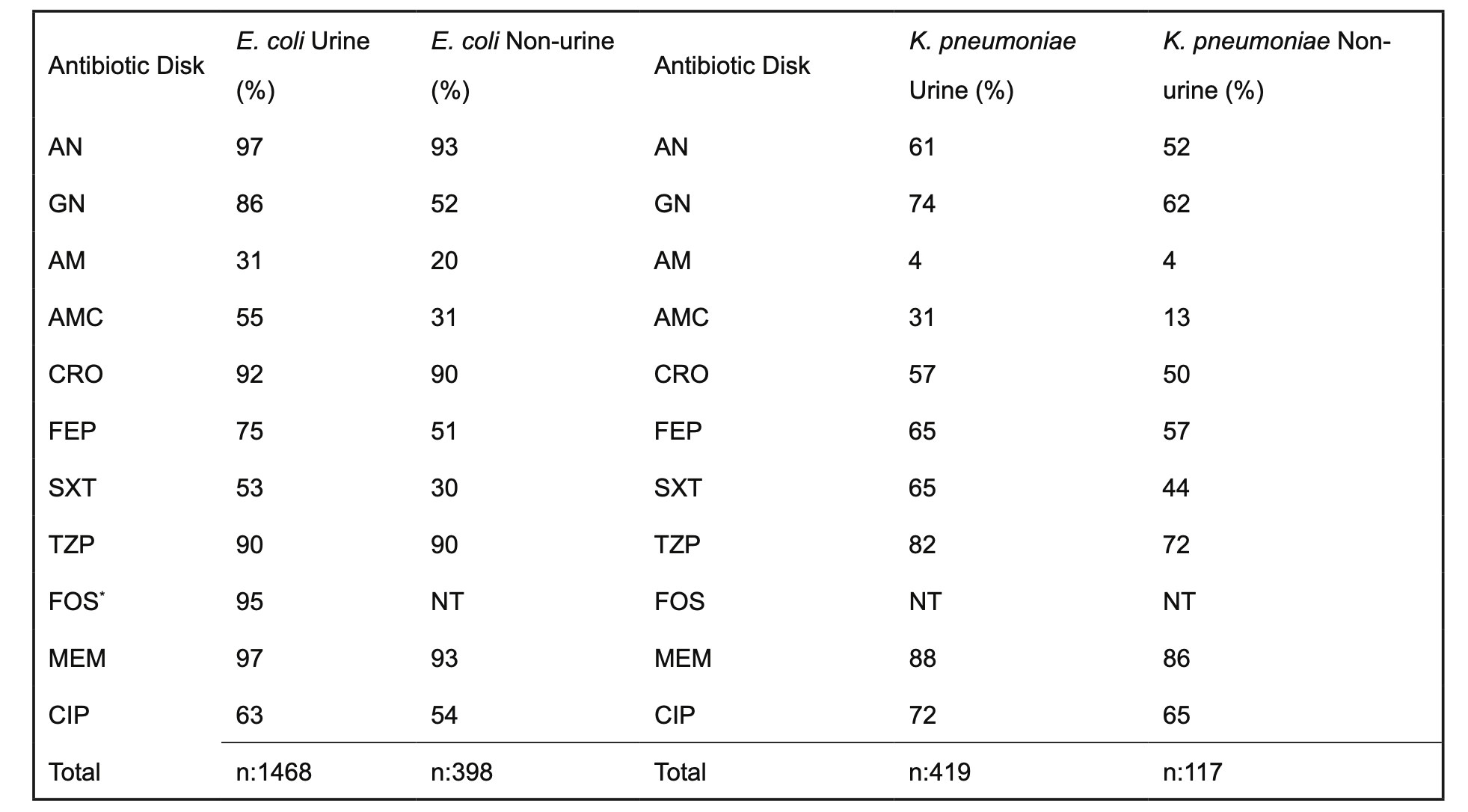
Objectives: This study presents antibiotic susceptibility data for Escherichia coli (E. coli) and Klebsiella pneumoniae (K. pneumoniae) isolates obtained from our hospital between January 1, 2020, and December 31, 2022.
Methods: Over this three-year period, we analyzed the annual antibiograms and extended-spectrum beta-lactamase (ESBL) positivity rates of E. coli and K. pneumoniae isolates recovered from urine and non-urine clinical specimens submitted to the clinical microbiology laboratory. Only isolates identified as causative agents of infections in adult patients were included in the analysis. The data were stratified based on sample type into urinary and non-urinary specimens, the latter comprising blood, respiratory, and cerebrospinal fluid (CSF) samples. Antibiotic susceptibility testing was performed using both the disk diffusion method and the VITEK2 Compact automated system (bioMérieux, France). ESBL production was detected via double-disk synergy testing and the automated system. Antibiogram quality control was routinely conducted on a monthly basis.
Results: A total of 4129 E. coli and 1385 K. pneumoniae isolates were included. Overall, the ESBL positivity rate was found to be 21% for E. coli, 33.2% for Klebsiella spp. Over the three-year period, E. coli isolates exhibited susceptibility rates exceeding 80% for carbapenems, aminoglycosides, ceftriaxone, and fosfomycin.
Conclusion: In conclusion, determining antibiotic susceptibility rates and ESBL positivity rates for frequently isolated pathogens such as E. coli and K. pneumoniae is of critical importance. It is imperative that healthcare institutions conduct these analyses at regular intervals in accordance with national and international guidelines and share the findings with relevant stakeholders. These efforts will make significant contributions to local and national antimicrobial stewardship programs and serve as a crucial guide for empirical treatment strategies within healthcare settings.
References
Baddal B, Güler E, Süer K. Antibiotic resistance in hospital- and community-acquired Pseudomonas aeruginosa isolates: The current status in Northern Cyprus. Turk Klin Mikrobiyol Infeks Hast Derg. 2024;34(1):10-15.
Akıllı FM, İlki A. Evaluation of colistin susceptibility in carbapenem-resistant Acinetobacter baumannii isolates using broth microdilution, MICRONAUT-MIC-Strip, and VITEK MS. MicrobiologyOpen. 2025;14(4):e70046. https://doi.org/10.1002/mbo3.70046
de Kraker ME, Stewardson AJ, Harbarth S. Will 10 million people die a year due to antimicrobial resistance by 2050? PLoS Med. 2016;13(11):e1002184. https://doi.org/10.1371/journal.pmed.1002184
Gajic I, Kabic J, Kekic D, Jovicevic M, Milenkovic M, Mitic Culafic D, Trudic A, Ranin L, Opavski N. Antimicrobial susceptibility testing: A comprehensive review of currently used methods. Antibiotics (Basel). 2022;11(4):427. https://doi.org/10.3390/antibiotics11040427
Yamin D, Uskoković V, Wakil AM, Goni MD, Shamsuddin SH, Mustafa FH, et al. Current and future technologies for the detection of antibiotic-resistant bacteria. Diagnostics (Basel). 2023;13(20):3246. https://doi.org/10.3390/diagnostics13203246
Ferrara F, Castagna T, Pantolini B, Campanardi MC, Roperti M, Grotto A, et al. The challenge of antimicrobial resistance (AMR): current status and future prospects. Naunyn Schmiedebergs Arch Pharmacol. 2024;397(12):9603-9615. https://doi.org/10.1007/s00210-024-03318-x
De Oliveira DMP, Forde BM, Kidd TJ, Harris PNA, Schembri MA, Beatson SA, et al. Antimicrobial resistance in ESKAPE pathogens. Clin Microbiol Rev. 2020;33(3):e00181-19. https://doi.org/10.1128/CMR.00181-19
Denissen J, Reyneke B, Waso-Reyneke M, Havenga B, Barnard T, Khan S, et al. Prevalence of ESKAPE pathogens in the environment: Antibiotic resistance status, community-acquired infection and risk to human health. Int J Hyg Environ Health. 2022;244:114006. https://doi.org/10.1016/j.ijheh.2022.114006
Rawat D, Nair D. Extended-spectrum β-lactamases in Gram-negative bacteria. J Glob Infect Dis. 2010;2(3):263-274. https://doi.org/10.4103/0974-777X.68531
Akpaka PE, Vaillant A, Wilson C, Jayaratne P. Extended spectrum beta-lactamase (ESBL) produced by Gram-negative bacteria in Trinidad and Tobago. Int J Microbiol. 2021;2021:5582755. https://doi.org/10.1155/2021/5582755
Castanheira M, Simner PJ, Bradford PA. Extended-spectrum β-lactamases: An update on their characteristics, epidemiology and detection. JAC Antimicrob Resist. 2021;3(3):dlab092. https://doi.org/10.1093/jacamr/dlab092
GBD 2021 Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance 1990-2021: A systematic analysis with forecasts to 2050. Lancet. 2024;404(10459):1199-1226. https://doi.org/10.1016/S0140-6736(24)01867-1
Salam MA, Al-Amin MY, Salam MT, Pawar JS, Akhter N, Rabaan AA, et al. Antimicrobial resistance: A growing serious threat for global public health. Healthcare (Basel). 2023;11(13):1946. https://doi.org/10.3390/healthcare11131946
Morency-Potvin P, Schwartz DN, Weinstein RA. Antimicrobial stewardship: How the microbiology laboratory can right the ship. Clin Microbiol Rev. 2016;30(1):381-407. https://doi.org/10.1128/CMR.00066-16
World Health Organization (WHO). Antimicrobial stewardship programmes in health-care facilities in low- and middle-income countries: a WHO practical toolkit. Geneva: World Health Organization; 2019. Available from: https://apps.who.int/handle/9789241515481-eng.
Lanckohr C, Bracht H. Antimicrobial stewardship. Curr Opin Crit Care. 2022;28(5):551–556. https://doi.org/10.1097/MCC.0000000000000967.
Karacaer Z, Filiz M, Yalçı A, Artuk C, Avcı İY. Determination of empiric antibiotic therapy in community-acquired complicated urinary tract infection. J Ankara Univ Fac Med. 2020;73(1):36-41. https://doi.org/10.4274/atfm.galenos.2020.59389.
World Health Organization Regional Office for Europe. (2022). Central Asian and European Surveillance of Antimicrobial Resistance: external quality assessment results 2020. Copenhagen: WHO Regional Office for Europe. https://apps.who.int/iris
Zhou Y, Zhou Z, Zheng L, Gong Z, Li Y, Jin Y, Huang Y, Chi M. Urinary tract infections caused by uropathogenic Escherichia coli: Mechanisms of infection and treatment options. Int J Mol Sci. 2023;24(13):10537. https://doi.org/10.3390/ijms241310537.
Duran H, Çeken N, Kula Atik T. İdrar kültüründen izole edilen Escherichia coli ve Klebsiella pneumoniae suşlarının antibiyotik direnç oranları: Dört yıllık analiz. ANKEM Derg. 2020;34(2):41-7. https://doi.org/10.5222/ankem.2020.041.
Karamanlıoğlu D, Aysert-Yıldız P, Kaya M, Sarı N. Extended-spectrum β-lactamase production rates and antibiotic susceptibilities among Enterobacteriaceae isolated from urine. Klimik Derg. 2019;32(3):233-239. https://doi.org/10.5152/kd.2019.68.
Mostaghimi T, Shirafkan H, Nasrollahian S, Fayyazi A, Hatami M, Rajabnia M, Pournajaf A, Halaji M. Worldwide prevalence of extended-spectrum β-lactamase-producing uropathogenic Escherichia coli isolates among kidney transplant patients: a systematic review and meta-analysis. Le Infezioni in Medicina. 2023;31(4):466–475. https://doi.org/10.53854/liim-3104-5.
Şenol A, Yakupoğulları Y, Şenol F F. Toplum kökenli üriner sistem infeksiyonlarında genişlemiş spektrumlu β-laktamaz üreten Escherichia coli ve Klebsiella spp. ve antimikrobiyal dirençleri. Klimik Dergisi. 2020;33(2)
Bozok T, Öztürk A. Niğde ilinde üçüncü basamak bir hastaneden izole edilen bakterilerin tür dağılımı ve antibiyotik duyarlılıkları: üç yıllık değerlendirme. Mersin Üniversitesi Sağlık Bilimleri Dergisi. 2023;16(1):22-39.
Bayraktar B, Pelit S, Bulut ME, Aktaş E. Trend in antibiotic resistance of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae bloodstream infections. Sisli Etfal Hastan Tip Bulteni. 2019;53(1):70–75. https://doi.org/10.14744/SEMB.2018.60352.
Castanheira M, Kimbrough JH, DeVries S, Mendes RE, Sader HS. Trends of β-lactamase occurrence among Escherichia coli and Klebsiella pneumoniae in United States hospitals during a 5-year period and activity of antimicrobial agents against isolates stratified by β-lactamase type. Open Forum Infect Dis. 2023;10(2):ofad038. https://doi.org/10.1093/ofid/ofad038.
Akıllı FM, Akıllı B, Ergan B. Investigation of antibiotic resistance rates of bacteria causing urinary system infection. Bozok Tıp Dergisi. 2025;15(2):155-161.
Semerci Z, Akıllı FM, İlki A. Evaluation of fosfomycin susceptibility testing methods: a focus on multidrug-resistant Klebsiella pneumoniae using ECOFF values. J Infect Chemother. 2025;31(4):102643. https://doi.org/10.1016/j.jiac.2025.102643
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Fatih Mehmet Akıllı

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.